Association of Mortality with Neuromuscular Blockade Differs According to Baseline Diaphragm Thickness.
Dianti J, Bertoni M, Goligher EC. Monitoring patient-ventilator interaction by an end-expiratory occlusion maneuver. Intensive Care Med. 2020 Jul 4:1–4. doi: 10.1007/s00134-020-06167-3. Epub ahead of print. PMID: 32623476; PMCID: PMC7334114.
Monitoring patient-ventilator interactions represents a key aspect when caring for patients receiving mechanical ventilation. Despite the numerous benefits of maintaining spontaneous breathing, vigorous respiratory efforts can worsen lung injury in patients with acute respiratory failure. Inspiratory effort can be monitored by performing an end-expiratory airway occlusion (Pocc). This represents a simple, non-invasive maneuver, that can be used to estimate excessive respiratory effort, dynamic mechanical lung stress, and can aid in differentiating various patient-ventilatory dyssynchrony.
Monitoring patient-ventilator interaction by an end-expiratory occlusion maneuver.
Dianti J, Bertoni M, Goligher EC. Monitoring patient-ventilator interaction by an end-expiratory occlusion maneuver. Intensive Care Med. 2020 Jul 4:1–4. doi: 10.1007/s00134-020-06167-3. Epub ahead of print. PMID: 32623476; PMCID: PMC7334114.
Monitoring patient-ventilator interactions represents a key aspect when caring for patients receiving mechanical ventilation. Despite the numerous benefits of maintaining spontaneous breathing, vigorous respiratory efforts can worsen lung injury in patients with acute respiratory failure. Inspiratory effort can be monitored by performing an end-expiratory airway occlusion (Pocc). This represents a simple, non-invasive maneuver, that can be used to estimate excessive respiratory effort, dynamic mechanical lung stress, and can aid in differentiating various patient-ventilatory dyssynchrony.
Figure. Representative tracings showing A) the airway occlusion maneuver in a spontaneously breathing patient at rest, and B) two patients with double triggering; one resulting from reverse triggering and the other resulting from a dissociation between neural and mechanical inspiratory time. Airway pressure (Paw), flow, esophageal pressure (Pes) and transpulmonary pressure (PL) were recorded during the expiratory occlusion maneuver. Pocc represents the inspiratory swing in airway pressure against an occluded airway. ∆Pes represents the dynamic esophageal pressure inspiratory swing. The dynamic transpulmonary driving pressure (∆PL,dyn) represents the dynamic mechanical stress applied to the lung during inspiration. By applying previously validated correction factors, clinicians can use Pocc to estimate respiratory muscle effort (Pmus) and ∆PL,dyn. In panel B, during the expiratory hold, there is no respiratory effort from the patient with reverse triggering, signifying that the double triggering is occurring in the absence of spontaneous respiratory drive. Conversely, an inspiratory effort can be seen during the hold in the other patients’ tracing.
Lung and Diaphragm-Protective Ventilation
.
Goligher EC, Dres M, Patel BK, Sahetya SK, Beitler JR, Telias I, Yoshida T, Vaporidi K, Grieco DL, Schepens T, Grasselli G, Spadaro S, Dianti J, Amato M, Bellani G, Demoule A, Fan E, Ferguson ND, Georgopoulos D, Guérin C, Khemani RG, Laghi F, Mercat A, Mojoli F, Ottenheijm CAC, Jaber S, Heunks L, Mancebo J, Mauri T, Pesenti A, Brochard L; Pleural Pressure Working Group, Acute Respiratory Failure Section of the European Society of Intensive Care Medicine. Lung and Diaphragm-Protective Ventilation. Am J Respir Crit Care Med. 2020 Jun 9. doi: 10.1164/rccm.202003-0655CP. Epub ahead of print. PMID: 32516052.
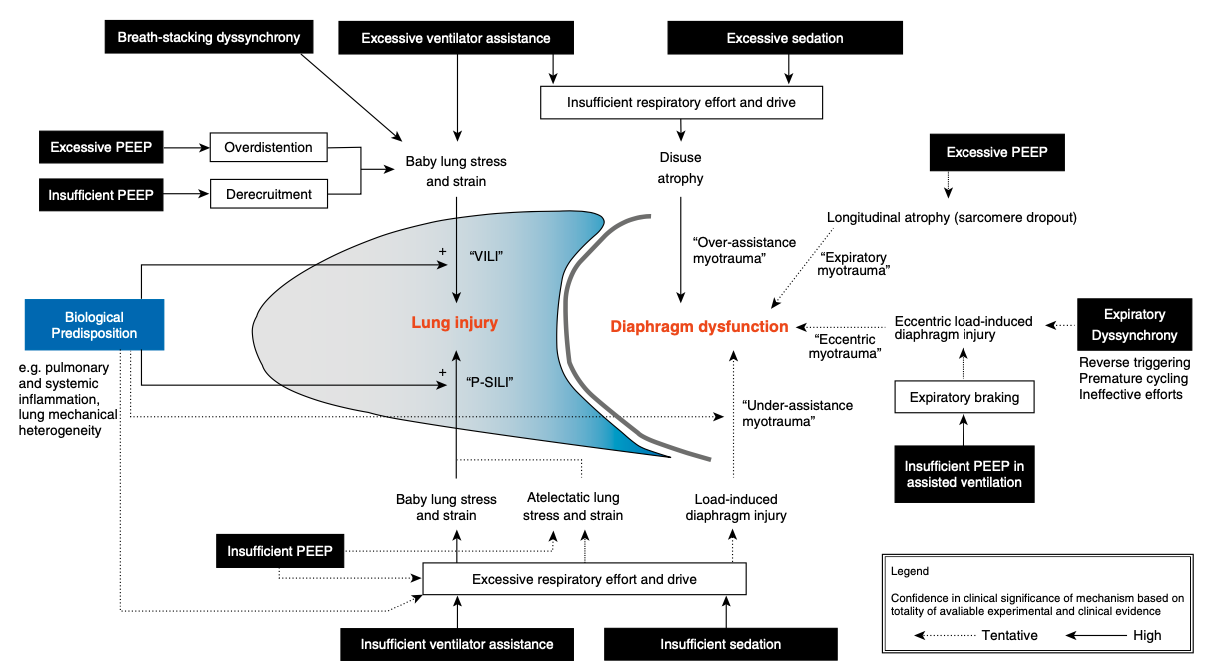
Lung injury primarily occurs as a result of mechanical stress and strain. Diaphragm atrophy and myotrauma occurs as a result of overassistance and underasssistance myotrauma. This Perspective proposed an approach called lung-and diaphragm-protective ventilation (LDPV) that aims to prevent ventilator induced diaphragm atrophy, injury, and weakness while maintaining lung-protective ventilation. This may be achieved by targeting low levels of patient respiratory effort simultaneously with safe levels of lung stress. Lung protection remains the priority. Trials are required to determine if this strategy can be effectively implemented clinically and if it can improve outcomes for patients who require mechanical ventilation
Association of Low Baseline Diaphragm Muscle Mass With Prolonged Mechanical Ventilation and Mortality Among Critically Ill Adults.
Sklar MC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, Rittayamai N, Harhay MO, Reid WD, Tomlinson G, Rozenberg D, McClelland W, Riegler S, Slutsky AS, Brochard L, Ferguson ND, Goligher EC. Association of Low Baseline Diaphragm Muscle Mass With Prolonged Mechanical Ventilation and Mortality Among Critically Ill Adults. JAMA Netw Open. 2020 Feb 5;3(2):e1921520. doi: 10.1001/jamanetworkopen.2019.21520. PMID: 32074293.
Diaphragm weakness in mechanically ventilated patients is correlated with elevated risk of prolonged ventilation, intensive care unit (ICU) readmission and death up to one year after ICU discharge. This study demonstrated that reduced baseline diaphragm thickness is independently associated with prolonged mechanical ventilation and ICU admission and a greater risk of in-hospital death. These data suggest that rehabilitation strategies that increase diaphragm muscle mass and strength might improve outcomes for patients in whom mechanical ventilation can be anticipated (e.g., major surgery, transplantation, high risk cancer patients).
Diaphragmatic
myotrauma: a mediator of prolonged ventilation and poor patient outcomes in acute respiratory failure.
Goligher EC, Brochard LJ, Reid WD, Fan E, Saarela O, Slutsky AS, Kavanagh BP, Rubenfeld GD, Ferguson ND. Diaphragmatic myotrauma: a mediator of prolonged ventilation and poor patient outcomes in acute respiratory failure. Lancet Respir Med. 2019 Jan;7(1):90-98. doi: 10.1016/S2213-2600(18)30366-7. Epub 2018 Nov 16. PMID: 30455078
There are several mechanisms through which mechanical ventilation may cause diaphragm injury and weakness. These include ventilator over-assistance (suppressing respiratory effort), under-assistance (inadequate unloading of respiratory muscles), eccentric loading (muscular loading during muscular lengthening), and end-expiratory shortening. In this paper, new data from mediation analysis is presented in support of the hypothesis that diaphragm myotrauma is an important mediator of the effect of mechanical ventilation on clinical outcome.
Mechanical Ventilation- induced Diaphragm Atrophy Strongly Impacts Clinical Outcomes.
Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, Vorona S, Sklar MC, Rittayamai N, Lanys A, Murray A, Brace D, Urrea C, Reid WD, Tomlinson G, Slutsky AS, Kavanagh BP, Brochard LJ, Ferguson ND. Mechanical Ventilation- induced Diaphragm Atrophy Strongly Impacts Clinical Outcomes. Am J Respir Crit Care Med. 2018 Jan 15;197(2):204-213. doi: 10.1164/rccm.201703-0536OC. PMID: 28930478.
During the early stages of mechanical ventilation, diaphragm atrophy/injury can develop. In this study we show that the changes in diaphragm thickness during mechanical ventilation are associated with poor clinical outcomes including prolonged ventilation and prolonged ICU admission. Modifying mechanical ventilation to prevent diaphragm atrophy and injury might therefore accelerate recovery from respiratory failure and improve long-term outcomes.